Safe Ways To Treat Chronic Pain Amidst The Opioid Epidemic

For someone suffering from chronic pain, even simple daily tasks can feel like arduous chores. From crushing joint, muscle or bone aches to psychological side effects like depression, it’s no surprise that results from the National Survey on Drug Use and Health revealed nearly 38 percent of adults in the US were prescribed opioids in 2015. But after President Trump declared the opioid epidemic a national public health emergency, alternative treatments for chronic pain may be put into motion sooner rather than later.
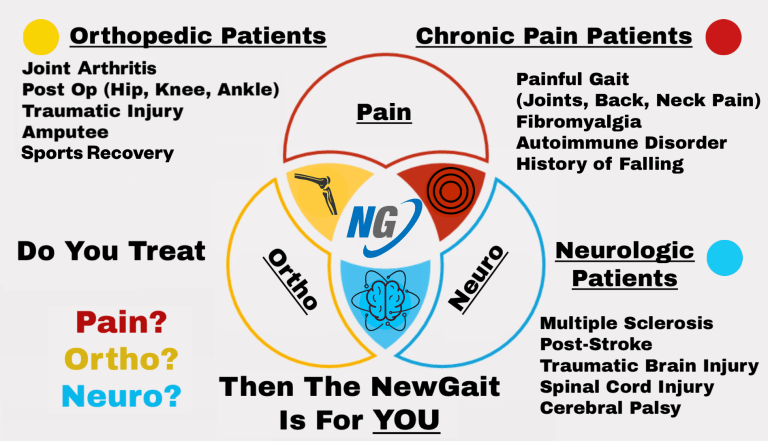
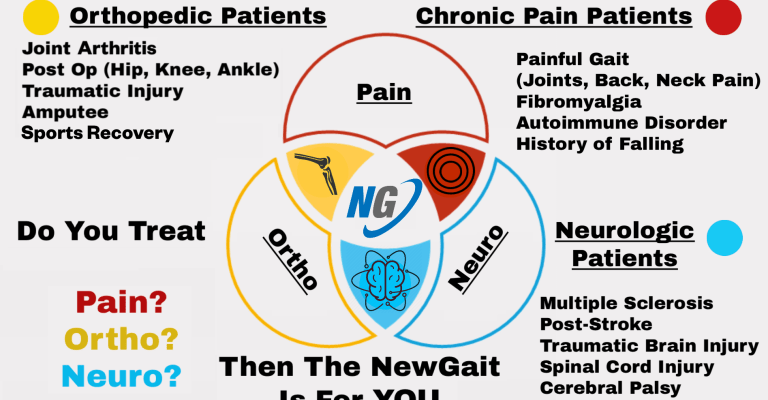
Regardless of the future of opioids, NewGait offers some suggestions for managing chronic pain a safe way.
Why Opioids are Dangerous
Aside from side effects like nausea, confusion, depression, sleepiness, and a decrease in sex drive, those using opioids are at risk for addiction and dosage increase due to tolerance development. Even more alarming, provisional counts from the Centers for Disease Control and Prevention show that 45,788 people died from opioids over a 12-month period ending in January of 2017. One need not be an addict or abuse the drug to put themselves at risk, which is what makes safer alternatives a more desirable form of treatment.
Don’t Neglect Mental Health

The mental side effects are just as taxing as the physical — especially if it’s the patient’s first time experiencing discomfort via illness or injury. Clinical studies showcased evidence that mindfulness meditation can reduce chronic pain by 57 percent — over 90 percent if the participant has previous meditation experience. Remarkably, photos of the brain taken during meditation reflect calmer brain patterns that continue to improve with treatment. It’s because of positive results like these that hospital-affiliated pain clinics can prescribe this type of therapy to help patients cope with mental health in relation to chronic pain.
Oftentimes, anxiety and depression accompany chronic pain. Fortunately, there are other methods that can help with these side effects and they include psychotherapy, pet therapy, massage, yoga, art and music therapy, yoga, and tai chi. Physical activity may seem like the last thing someone in pain may want to do, but some exercise — even minimal — provides a natural painkiller because the body produces hormones called endorphins that work to increase pain tolerance, while endorphins unite with brain receptors to alter one’s perception of pain.
Find Ways to Reduce Stress and Anxiety
Anyone with chronic pain understands that stress and anxiety can often cause flare-ups, which, in turn, make stress and anxiety that much worse. If you find it difficult to clean your house, or the amount of clutter in your living space has gotten out of control, take steps to correct the problem. In addition to bringing in a cleaning service to give your home some TLC, you can also put some of your unused furniture into storage so you’ll have more space — and less clutter.
There are also some simple steps to take to help mitigate stress found at the workplace, an especially — and unfortunately, common — aspect of the job for those in leadership positions. One strategy is to replicate those who seem to be keeping their heads while others are losing theirs during trying periods. Sit down with them when things are calm and find out what their thought processes are, and be intentional about incorporating the same methods when trouble comes calling.
Try out a natural remedy
While it may be hard to get used to accepting natural remedies for chronic pain after taking prescription medication, research has proven that there are effective alternatives with virtually no side effects.
While it may be hard to get used to accepting natural remedies for chronic pain after taking prescription medication, research has proven that there are effective alternatives with virtually no side effects. For example, a study conducted by the American Association of Naturopathic Physicians revealed that after 75 days of taking fish oil — an anti-inflammatory supplement — more than half of the 125 patients in the study stopped using their prescription painkillers. Turmeric is another anti-inflammatory supplement that has been proven to be effective.
Researchers found that the resveratrol found in berries and red wine (in moderation) works on a cellular level to regulate pain. On a more traditional level, old-school heat and cold therapies (think hot Epsom salt bat
Acceptance

No matter what path to relief a patient chooses, it’s helpful if acceptance is incorporated into a chronic pain treatment plan — particularly where mental health is concerned. Finding ways to manage the pain both physically and mentally can create the foundation for navigating this diagnosis and give you a better sense of control.