NewGait CEO, Benga Adeeko, had the opportunity to ask Cathy Ruprecht, PT, NewGait Clinician, and pain specialist, a number of questions regarding the treatment of chronic pain, and how The NewGait has changed the way she practices. Also features Kim Spranger, PT and NewGait Clinician
Watch the video version here. Cathy Ruprecht, NewGait Clinician and Physical Therapist, gives us an in depth discussion regarding chronic pain. Moderated by Benga Adeeko, NewGait CEO. Also features Kim Spranger, PT & NewGait Clinician.
CATHY: My colleague at the time, Kim Spranger, had just come across this product, and was using it with a client. One day brought it out, dumped it onto the table and said, “Look at this neat thing that I have here. Let’s try it and see what we can do with this, because I think this has great potential to help people.” So I looked at it and I said, “Ok…I’m game.” So we started to use it with clients in the clinic and four years later now, it’s been quite an evolution and revolution in our practices.
CATHY: Well, chronic pain is how we classify pain that is long term and persistent. Usually when someone has an accident or an injury or surgery, there is some sort of a tissue damage. It is usually repaired in about three months. Most people heal right up and go on about their business, and they don’t have much pain at all remaining. But in some individuals, pain is persistent and can linger for years after someone has had an accident or injury. We’ve also learned that pain can come on without an accident or an injury of some significant level of tissue damage, and so these individuals find this pain to be life-changing and very disturbing for them, so my job is to try to teach them about pain and get them moving again, and that’s been the journey that I take them on. We have now in recent times begun to look at pain a bit differently. We always equated tissue damage with pain, but we’ve now learned that some individuals have no tissue damage and significant levels of pain, some people have significant tissue damage and no pain, and so pain is very complex and we now define it, instead of a biomechanical model, we now look at it as a bio-psychosocial model where there are many aspects of our emotion and our memory and our brain thought processes that contribute to someone’s pain experience.
KIM: I would like to add to that, you know, Cathy’s journey with chronic pain has been very interesting. In the 1990s we were asked to get involved with developing a chronic pain program for our region. Cathy took it to a totally different level and actually in the last couple of years, she has developed a long-term philosophy on how to treat chronic pain that all of us have now adopted and are using in our clinics. I think of a patient this fall who came back and she said, “This has changed my life. I want you to know how much you’ve changed my life by the way that you’ve approached my pain.” So I want to give a whole lot of credibility to what Cathy is saying and she has changed the way we are treating chronic pain across the upper peninsula of Michigan.
CATHY: Many individuals have been to multiple doctors over time and have had multiple procedures done, for which their pain seems to be unrelenting and ongoing, and at that point, sometimes the physicians will say, “Well, this looks like a chronic condition for you. We don’t see anything that’s life-threatening. We don’t see anything that needs surgery or operations, you’re medically stable, so at this point we are going to diagnose you as having chronic or persistent pain and perhaps a different approach for therapy may be helpful for you.” That’s oftentimes how people find their way to me.
CATHY: What I practice is pain is not just a tissue damage issue, so people come in, they bring their minds, they bring their thoughts, they bring their ideals, they bring their beliefs, they bring this history of their pain and so with the practice that I use, it’s a bio-psychosocial model of pain, so we look at pain in multiple levels as far as what’s your stress level like, are you getting good sleep, what other aspects of your health might be contributing to your long-term pain and how might we utilize those aspects to help you change and regain control of your pain, so oftentimes I’m not there to try to change pain…I will explain it…I don’t have the magic exercise, I don’t have the magic power in my hands to take your pain away right now, but we’re going to recognize and build on that you’re medically stable and that what you have you can do things with and over the course of time as you increase your activities and as you start to lose some of your focus on the pain, you’ll find that it does become less intense and less frequent and less debilitating as we move forward in this different way to look at pain, and so I spend a lot of time working with people on body awareness. Many people when they have chronic and persistent pain, they really don’t have a great mind/body connection. They’re not very aware of where they are in space. They really view sometimes their own body as the enemy. They don’t want to think about it. All it is, is a source of pain and so I try to reconnect them to their whole self and that’s the fun of what I get to do, so we work on all sorts of aspects; use of mirrors to see where we are in space, focusing on movement patterns that are comfortable, body parts that don’t hurt, and so I have a whole toolbox of things that we go through and teach, but we also really try to work on understanding lifestyle’s contribution to pain, anxiety’s contribution to pain, fear and worry and anxiety’s contributions to pain, and so we want to try and break this cycle of how someone might be living by giving them something new and different to do that then will allow them to move forward with less frequent, less intense pain.
CATHY: You know, each therapist develops their own beliefs and their own toolbox in working with folks with chronic and persistent pain, for instance, someone comes to me with back pain. Typically, a therapist might do some manual therapy on them, massage, electrical stimulation, certain exercises to build the core, that kind of thing. But my philosophy is to spend a lot of time on education, on really understanding the nervous system, how they function to keep us safe and then how that nervous system can be manipulated through some tools like your breathing can change the way your body is perceiving itself and to create changes within our nervous system’s connections to the brain, and so what I do is a lot of education, a lot of mindfulness, a lot of breathing and, again, body awareness, and so we try to build different tools into a box that a patient might not have seen before because many times when a patient comes to me, they’ll say, “Well, I’ve been to therapy before,” you know, and “been there, done that. What are you going to do that’s different,” so in order to really do something different, I have to have something different, and so that’s one of the tools that I use is the NewGait because that also is something new and different in helping people with chronic and persistent pain.
CATHY: I wish I knew exactly. If anybody wants to do some research, call me… but I have some ideas and some theories on it and taking what I know and combining it with what I see, and so there are a couple of things that I really have some strong opinion and belief about — there’s a woman named Amy Cuddy…she’s a Ph.D., and if you’re not familiar with her, she’s written a book called Presence. She has this fabulous Ted Talk on YouTube about posture, and in her Ted Talk, she talks about our bodies and our minds, and she says that our bodies change our minds, our minds change our bodies, and our minds change our behaviors, and our behaviors can change our outcome, and to me that’s a really very powerful statement, and, in that, when we walk, walking is a really important component for treatment of chronic pain. When we walk and when we do cardiovascular exercise, it changes our blood flow, it changes all sorts of physiological responses within us, and for many people with chronic and persistent pain, it can really help to decrease their level of their pain, and so when you have people with chronic and persistent pain, the last thing they typically want to do is go for a walk and so the NewGait allows me to make some changes in how they walk, it allows me to change their postures, and so by changing our postures — Amy Cuddy again, relating back to her — has done a lot of research to show that when we change our posture into a more powerful, upright, balanced alignment, we really are changing our body’s physiology. We’re decreasing cortisol and stress levels. There’s a powerfulness that almost feels like it exudes from you when you change your postural alignment and positioning, and the NewGait, by putting it on, it gives my own self…plus what I hear from my clients…it gives us a sense of grounding, if you will, or a sense of scapular depression is what I often feel, and I feel myself draw taller, and when I do that…and from what Amy has stated in her research…we are making a change in our physiology, and any time we can decrease stress and cortisol levels, we’re also then able to change the nervous system to a more relaxed, comfortable positioning, and so therefore then many clients report that they feel less pain, and that has been a really interesting and rather unexpected benefit of the NewGait’s use with clients and patients is when they literally turn to me and say, “I walk now and I don’t have any pain,” and that was really not something I had anticipated or expected, but I tell you, when I heard it the first two or three times from patients, I said, “Wow. There must be something going on here,” and so that’s when I really started to embrace the NewGait as a device to help change peoples’ movement patterns. Many people when they come in with persistent and chronic pain, they have a really distinct posture. They are very withdrawn, pulled in, pulled down, and so if you change physiologically by straightening and being taller and standing and occupying more space, then that’s a huge benefit again in pain management, plus when I put people into the NewGait, I also believe there are some other factors happening. I recently read a book called Explain Pain by Lorimer Moseley and David Butler, and they had some ideas which I grabbed a hold of when I read through that also then relate to the NewGait for me. A couple of things that they had said was, you know, your body, your sensory system, your nervous system, is reporting constantly to your brain different things. It senses temperature, it senses mechanical pressures and stimulations, and it senses chemistry within you so, certainly, when we are in a state of stress, then we are going to have more bombardment of those stress hormones and that can, again, elevate someone’s pain, so when we are able too change physiologically their posture, that, to me, is soothing for the nervous system. The other thing about the NewGait is it creates a joint congruence and once again, relating back to explaining pain, when we have joint congruence and there is an approximation increase at the joint, specifically I feel it through the scapula and at he hip joint at the greater trochanteric joint, when I experience that sense, my body feels more calm from that congruence, and also when we’re in a stress state, we also tend to operate with our bigger, extrinsic musculature because we’re going to heighten state of arousal, ready for flight or fight, but when we’re able to become more relaxed and more confident within our bodies, the smaller intrinsic muscles like your multifidus and your postural control muscles and your ability to breathe deeper with your diaphragm, is also changed and the body finds that calming as well, so there is definitely, from the NewGait, a sense of deep pressure hug. You feel it around your thighs and calves from the limb strap, from the shoulder harness, from the waist strap, that’s changing sensory input to the brain and that then is what I believe is giving people a sense of decreased pain as they move through space. What’s been interesting is also how people move with chronic pain, their gait pattern. You see a real lateral, side-to-side gait pattern. Their movements are slow and guarded. They’re usually dragging along some sort of a limb, so oftentimes I see people who have had knee pain, hip pain, back pain. They might have piriformis syndrome where they’ve got a lot of gluteus maximus pain in that region. They also might have some sort of sensory impairment like they’ve lost dorsiflexion or they’ve lost their ability to push-off/toe-off, and they’ve got no power in those gastrocs to push off. Well, every time you bring your leg forward into swing phase, that creates this lurching motion, but with the NewGait, I can change that. I can change their step width to make them more balanced. I can change the ease with which they get hip flexion, I can give them a quicker break-over at the ankle for a faster push-off at that toe-off moment to start the swing phase, and so it’s been really interesting to see the changes in gait. Again, with an improved posture, I can initiate trunk rotation and arm swing, and so the result of use of the NewGait with my chronic pain patients has been really quite remarkable, not only for me, but for them.
CATHY: I pretty much have it on everyone, at least…when people come to me, I really want to see how they move. I want to increase their walking confidence. I want to increase their walking speed. We know now that walking speed is indicative of someone’s longevity, and so I want to make changes in how they move because that is so essential to life. Walking and walking briskly to cover ground allows us to take our minds out to explore and it allows us to do the things we no longer have been doing because of our pain, and so I really focus a lot on gait and movement and walking as a treatment strategy, and so I videotape everyone. I get a walking test on them to see how fast they’re moving. I analyze that video. I look at their movement pattern and then we look at it together and they can see how they can move differently, and the cool thing is sometimes when we get the bands just right, and I don’t know exactly where that’s going to be. There are different configurations of the NewGait that I will apply, and what I’m looking for is that individual’s nervous system to tell us when we hit that eureka moment when they suddenly say to me, “Wow. I’m walking without pain,” or “Wow. My pain is down significantly from when I can in here,” and for some people, there is carry-over. They have less pain…it might be for an hour after they see me. Sometimes it’s three or four days after they see me, so there is a huge neurological change happening within them when they use this device, and so it…I don’t know exactly who that person’s going to be…for whom they break into tears and say, “Oh my gosh…I haven’t walked like this in years,” but if I don’t put it on someone, I won’t know who that person’s going to be and I may have missed an opportunity to really change their life and change their gait with this really unique tool that gives them a different feedback to give them a different output of their pain than they had experienced ever before.
CATHY: I let the clients guide me. They’ll come back and I’ll say, “How did you feel after you were here? What was your experience,” and many times they’ll say, “You know, I went to the grocery store and I walked or my family noticed I was walking differently, or my father said, ‘Oh my gosh. Look at your posture. Look how straight and tall you’re standing. Look at how fast you’re walking,’” and so I get their feedback, and if they feel like they are now doing better, they may not need it again. They have that change of perception in self that we were looking for…boom, we’re good to go, but sometimes they’ll say, “You know, I want to try that again. I can’t wait to get back in that because I felt so different, so much more powerful, so much more confident, like I could walk like I used to.” That’s what they’re looking for with me, so each person has their own response to it and I let them guide me.
CATHY: Well, what we work on then is body awareness, so we’ll go to the mirror and we’ll work on posture. We’ll work on balance in single limb stance. We’ll work on “Well, where are my shoulders, where is my levelness in my waist, how am I aligning myself,” and so we’ll look at all of these different changes that we’re trying to establish as they’re standing and trying to recreate a new sense of self. I’ll have them climb stairs. I’ll have them do step-ups. “Where is your weight, using your gluteus to give yourself a lift, think of the weight through the heel.” It’s a lot of, you know, “Where are you in space,” and so we work on proprioception again, both with the mirror, sometimes without the mirror. We’ll work with SportCord. I’ll have them do some upper body work with resistance bands while they’re stabilizing their posture, while they’re stabilizing the lower portion of their body while they’re wearing the NewGait. Sometimes we’ll go for a walk in the parking lot or, depending on the weather, we might go over some hill and dale, up and down some different levels of terrain, so we’re using it in the clinic to walk, we’re using it in the clinic to stand and reshape where we feel our body and, again, it’s that mind-body connection I think that’s helps people have a new perception of how they move, that they can move differently and by moving differently, they sometimes feel a whole lot better.
CATHY: Remember, many times, people have been to therapy elsewhere and so in order to try and provide something different, I will say, “Hey, I have this special suit that we can try and many people find it very helpful for teaching you about where you are in space and some people really love this to walk in and you might too find that it’s helpful for getting you to move like you used to, to move more comfortably and more confidently,” and so they’re so wonderful…they’re so wonderful to give it a try, and I tell them too, “You know, if you don’t want to or if this isn’t comfortable, you…you just have to tell me and we will be done, but let’s see how it feels because your body is going to give us a response just like it’s responding to the fact that it’s unhappy about something by giving you the perception of pain, right?” When we get it different, suddenly your body goes, “Hey, I’ve been waiting for a long time for you to change up the way you’ve been walking. Now I don’t have to report about that pain anymore,” and so we play with the…we’re really just manipulating the nervous system maybe and that’s what we do…we think of it as fun and it’s playful and I try to make it entertaining, and so they’re pretty game to give it a go, and the best ones are the ones that give you that skeptical eye…that they’re quite sure that you are just nuts and this isn’t going to make a change, but they’re the ones that are most rewarding, of course, because they’re the ones that go, “Wow. I didn’t expect that,” so that…that’s really…it’s a joyful day for me to go to work. It’s a joyful experience to get this on people and to do the magic that I get to do with them and share what I am so passionate about and to have them respond to it so positively.
CATHY: It’s been a very joyful experience…one of the most rewarding of my life, especially at this point in my career, so to be able to go to work and to bring to someone a sense of hope that their life can be different, and so that’s a pretty joyful experience right there, and so we’ve now taken the NewGait to some clinics and shared with other therapists while they have their own clientele there and to see the response from their own patients, to have a clinic of several therapists tearful and joyful. Literally, patients walk and blossom before your eyes. It’s almost for me a euphoric high. I mean I just can’t tell you how cool it is to be able to use something like this in a clinical setting and to have such a dramatic result in such a short amount of time. That’s just been a game-changer for me. It’s like putting on an erector set on someone and just manipulating a band here or trying a band there or working as a team with the other therapists and the patient’s input to just get the right combination to have that person move with ease and confidence, and it’s just been the most joyful thing.
KIM: I love how adaptable this is and how quick I can manipulate and change it. That is the absolute appeal of it to us clinicians is that you can be inspired and in a moment’s notice, you can react to your inspiration and change their world.
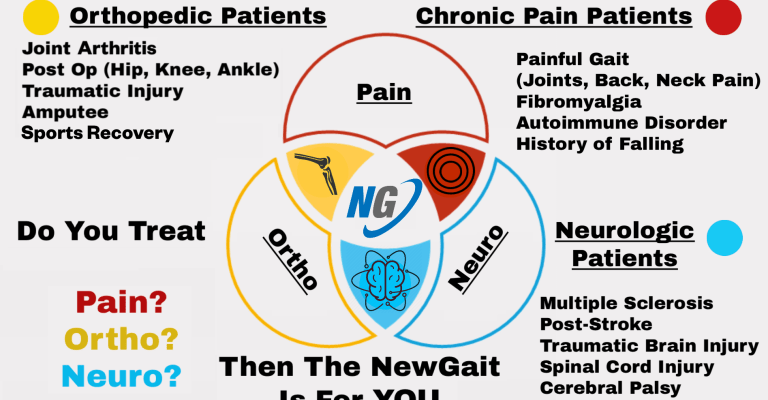
CATHY: The results are instantaneous. I mean, you put it on and they move three steps away from you and you can see the result of it. You don’t have to let them walk for five minutes or three days. You know instantly whether that band is right where you want it or not and if not, you just change it up and put it somewhere else and go with another option for the use of the device. But from…again, from a therapist’s perspective, from trying to really change walking, what tools have we had in the past. We’ve had Ace wraps and we’ve had some Thera-Band, but this…when you put this on as a therapist and you feel what this can do, you will be amazed…blown away…because then you’re going to know exactly like what patients…” Oh, I should have used this…I should call up so-and-so and have them come back. I’ve got this new tool. I bet I could manipulate that part of their gait pattern. It is just really fun, and sometimes therapists are a little intimidated by it, of course, because you want to do the right thing, but, you know, and sometimes we’re very analytical about it, like, “Well, I don’t know what muscle is not working. I need to put this right in the right places.” You know, sometimes I think I know what this person is going to need and I put it on and they go, “It’s not working for me,” so then I’ll go, “Okay. Let’s try this here. Let’s try this there,” and all of a sudden, boom…you get it, and so it is so easy to use. You can put the bands in any combinations and your client is going to give you immediate feedback on whether that was the way to go or not, and they, too, will offer suggestions like, “Well, what if we put a band here.” “Well, let’s try it,” and then, boom, off they go and they’re happy as a clam. So it has been, again, a really cool manipulative tool in the clinic that we’ve tried to use before, and there is research out there, even though this is a relatively new product and, boy, there is a lot more research I’d love to do, as with my partners, too, but there is research to support the use of Thera-Band in a gait-assisted pattern and this is, again, a Thera-Band type elastic band manipulation of movement, and so there are also different suits that have been designed over the years that we recently came across that also have support to show that this type of an idea is beneficial and this, again, this product is so easy to use, so affordable really for clients to purchase for home if they need it for long term. And the other things about chronic pain is people often say, “Well, but it’s chronic pain, you know…it’s not a neurological condition. It’s not an orthopedic condition.” Well, yeah, it is. My people often have orthopedic conditions. They’ve had knee replacements. They still have pain. They’ve had all sorts of surgeries on all sorts of body parts, fused ankles. They have had stroke. They’ve had failed back surgery. They’ve had MS. They’ve had all sorts of chronic and persistent pain from a multitude of neurological and orthopedic, and sometimes both, and this device has been able to help any and all of them, and so that’s what’s so cool about it.

Cathy graduated with her Master of Science Degree in Physical Therapy from Grand Valley State University in Michigan. After having worked in a variety of therapy settings for 20 years, Cathy discovered a passion for helping people with Chronic Pain. Cathy is using the NewGait daily with a variety of patient conditions after discovering how helpful the device can be.