Sciatica Rehabilitation

Welcome to the Topic “Sciatica rehabilitation”
Sciatica is a medical condition relating to the sciatic nerve branching from your lower back. The sciatic nerves branch throughout the lower half on both sides of your body. Therefore this medical condition only affects one side of your body.
The onset of sciatica occurs when the sciatic nerve is compressed, consequently causing inflammation, intense pain, and numbness in the affected side of the body. Sciatica can be quite a painful condition, and most patients struggle severely. However, rest assured; most patients quickly heal within a few weeks.
What to Know Before Rehabilitation
As mentioned earlier, sciatica cases are usually severe, but it is possible to treat them entirely in the span of a few weeks. The good thing about rehabilitation for sciatica is that treatment options are almost exclusively nonoperative. This means that the recovery path is generally focused on more natural treatments rather than surgeries.
That said, treatment may be necessary for specific situations. For instance, sometimes sciatica is not caused by any regular source, such as overworking oneself. In cases where the pain is caused by accident or injury, and it is basically impossible to perform essential functions such as walking or controlling your bladder, the condition may be severe enough to be operated on. Most of the time, specific treatments and rehabilitation therapies are more than enough to get the sciatica patient back on their feet.
Discussing the condition’s level with your health professional is crucial. Depending on the cause of sciatica, the treatment is likely to differ significantly. Sciatica caused by accidents is more of a concern and will likely involve operations. The patient must consult the details of the procedure with the professional at length, its pros and cons, its necessity, and what the process will involve.
Physical Rehabilitation

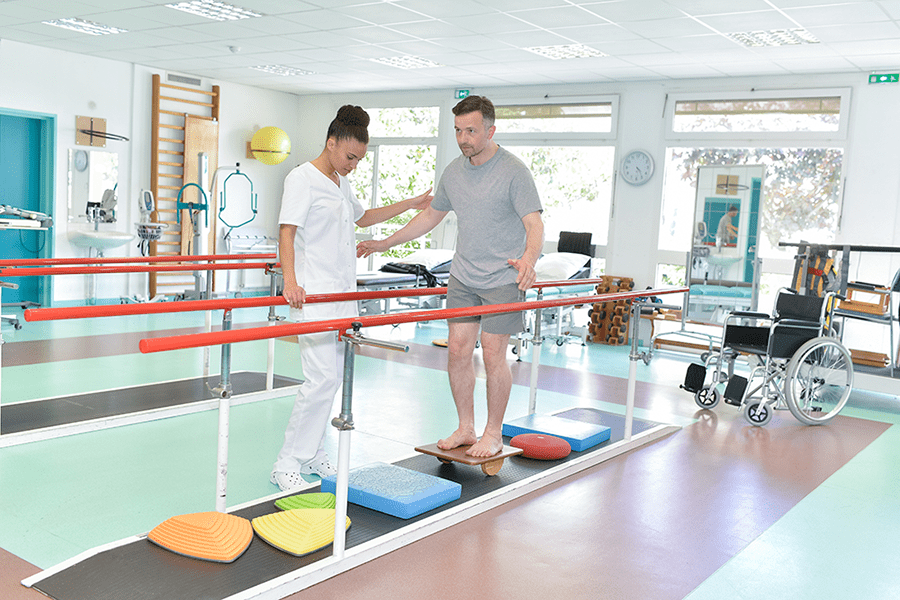
Considering the fact that pain caused by sciatica mainly results in physical issues, such as free and easy movement, it is not surprising that physical rehabilitation is the top priority for sciatica patients. Physiotherapy comprises the essential part of rehabilitation for sciatica patients with the goal of relieving them of their pain and preventing further symptoms. The main symptoms of this condition include pain across the body and even numbness in the lower part of the body; exercise, therefore, becomes a crucial part of treatment for sciatica.
Physiotherapists may focus on a variety of exercises that aim to lessen the patients’ pain and condition their muscles to withstand the condition. Extension and back exercises aim to relieve that pain by focusing on the movement of the spine. Additionally, the physiotherapist may facilitate the patient with strengthening exercises and joint mobilization to help them keep the lower part of the body active. While some doctors prescribe bed rest, it is best to counter this condition with activity and exercise. Exercising and moving according to the physiotherapist’s directions is the best path to recovery from sciatica.
One area where patients may struggle is with walking. For this, the physiotherapist may focus on gait and balance training. Once the muscles are strong enough to support the patient’s weight efficiently, the physiotherapist may help the patient train and relearn previous patterns for movement and walking.
Dry Needling
One therapy that is increasingly gaining more traction among health professionals is dry needling. Dry needling is a technique in which a small needle is used to pinpoint the area in a muscle that promotes movement. This technique is particularly beneficial if the patient is struggling with contracted muscles. Targeting the trigger point helps the muscle release the tension, and it ultimately reduces the pain. It must be noted that this form of therapy must be carried out by a certified health professional to ensure accurate needling and minimal side effects.
Chiropractic Therapy
Sometimes, the symptoms of sciatica may prevail, and the patient may have difficulty moving on their own for fear of pain. In such cases, the patient may require intensive care. A chiropractor may be involved in the recovery process. Chiropractic therapy involves manually manipulating the patients’ limbs to improve their spine’s alignment.
Chiropractic therapy is beneficial if the sciatica is not a result of injury or accident but instead caused by a herniated disc. It improves muscle strength, flexibility, and the range of the patient’s movements – all these are areas where a sciatica patient typically struggles. This therapy aims to prime a patient’s body to work at the best of its ability.
Occupational Therapy

Considering the repercussions of sciatica, it is not surprising that patients with sciatica struggle so much with daily activities. Even though the pain may be quite severe, it is recommended that the patient does not confine themselves to the bed for their recovery. Laying around all day will simply aggravate the symptoms because the body is not receiving the exercise and movement it desperately needs to keep the joints in working condition.
That said, it is also essential to keep in mind that despite the direction to continue daily activities and exercise as is, patients with sciatica will struggle more than other people to carry out these simple tasks. Therefore, they will likely require an occupational therapist to help them with their daily tasks and guide them to move accurately so as not to aggravate their symptoms and cause further pain. An occupational therapist may teach the patient specific techniques to move safely and helpful sleeping and resting postures to ease their pain.
Massage Therapy
Because sciatica is mainly a physical condition, massages are reasonably helpful in easing the patients’ pain. Massages are relaxing enough as is, but certain types of massages may be used for sciatica patients to relieve their pain and bring movement back into their numb limbs. Massages will facilitate blood circulation, leading to a higher healing rate within the body – this acts as a natural pain reliever. Furthermore, sciatica is also characterized by tightness and soreness in the muscles, for which massages will be ideal. Certified massage therapists should be involved in the process to ensure the patient’s highest level of care and safety.
Have any questions regarding the topic “Sciatica rehabilitation” feel free to comment below.
Also Read: Rehabilitation for epilepsy