Stroke Rehabilitation
Welcome to the Topic “Stroke rehabilitation ”
Strokes are very common medical issues, but few are aware of the exact symptoms, causes, or treatments. Strokes are basically attacks on your brain that may be caused due to a ruptured artery or a blocked artery within your body. Essentially, the blood supply meant to reach the specific part of the brain does not, leading that part to be damaged or, in more extreme cases, die. The consequences of a stroke are relatively severe and last throughout the patient’s life, making it a painful condition.
The brain is responsible for movements, memories, motor coordination, higher executive function, and controlling any communication between itself and the body. Therefore, any part of the brain being damaged also damages the body’s functions. Depending on the part that is damaged or dead, patients may experience several of the following common symptoms:
- Perception difficulties
- Confusion
- Difficulty seeing
- Severe headaches
- Difficulty in walking, talking, or moving as usual
- Slurred or grossly disorganized speech and movements
What to Know Before Rehabilitation
Any of these symptoms may occur immediately as the patient suffers the onset and well after the stroke has passed. There are several treatments and strategies for rehabilitation for stroke patients. However, for the most part, strokes prove to inflict long-lasting and irreversible damage on the patients. Rehabilitation for stroke patients begins immediately during the stroke, and the medical team may administer intensive care for the first few days. Afterward, rehabilitation teams may focus on easing the patients back into their lives and helping them adjust to their new condition seamlessly.
There is no time limit on recovery from a stroke; while some may recover within weeks, others may take months or may never fully recover. The path to recovery may differ for all stroke patients, so it is essential to be mindful of the patient’s prognosis when detailing rehabilitation treatments and therapies. Depending on the type of stroke and the recovery time, rehabilitation could look very different for the patients.
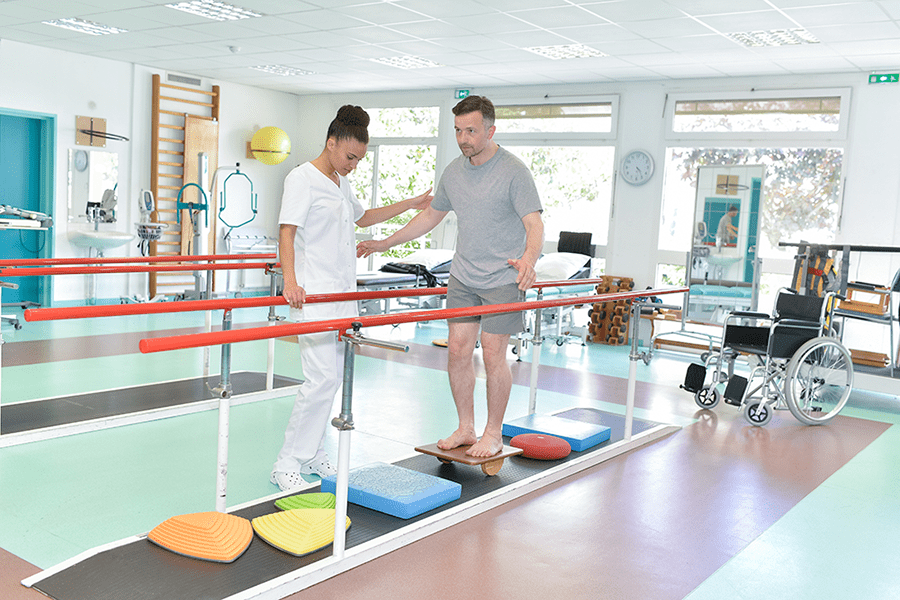
Physiotherapy

Physiotherapy is one of the essential parts of recovery treatments after a stroke. It is generally recommended that patients complete at least an hour of physiotherapy every day after their stroke – provided they are strong enough. However, most of the time, doctors may have higher expectations from patients who actually require more assistance than they first thought. Physiotherapy will tackle the patient’s issues with balance and stability, along with strength and flexibility training.
The stroke may have caused damage to neural connections, and to rebuild those connections, it is crucial to go back to step one and learn the most basic of functions, such as walking, standing, and moving your limbs at will with precision. Furthermore, stroke survivors may also have to deal with paralysis; most of the time, one side of the body is affected. Another part of physiotherapy is learning how to move and go about life even without using those paralyzed limbs.
Occupational Therapy
Occupational therapy in stroke rehabilitation will aid the patients in learning the skills needed to adjust to their new life and relearn some aspects they no longer remember. The most important task of an occupational therapist is to aid survivors in managing personal tasks independently; these include but are not limited to bathing, washing, feeding, using the bathroom, and everyday tasks. Further down the recovery path, occupational therapists may aid the patient in performing more complex tasks such as relearning to drive, cleaning their room, or preparing basic meals. All these tasks require perfect motor coordination, and the therapist is responsible for ensuring that the patient regains that coordination, strength, and balance to perform daily life functions.
Speech Therapy
As mentioned in the list of symptoms, stroke patients may also suffer from disorganized speech and difficulty in articulating. Stroke patients may also have trouble understanding other people. Here, speech therapists will be essential to their rehabilitation and recovery. Such issues with speech may also be categorized under “aphasia,” which speech therapists are equipped to treat. They may begin the treatment of the patient with the most foundational knowledge of pronunciation and phonics. Being patient with stroke survivors is essential because they will have varying times and levels of success. Eventually, stroke survivors may be able to regain their previous abilities to communicate through speech therapy.
Psychological Rehabilitation

Strokes can cause irreparable damage to the brain, and besides affecting the rest of the body, they mainly impact the higher executive functions of the affected individual. How a person forms thoughts, strings together concepts, plans, and organizes are all functions that are affected by the onset of the stroke. Rehabilitation must therefore include psychological counseling and treatment as well. Psychological rehabilitation may involve facilitating the patients dealing with depression and anxiety. Both these mental states will affect how the patient responds to the rest of the treatments. It is crucial to ensure that the patient is mentally healthy and motivated enough to handle the recovery process.
Electromechanical Assisted Training
With the constant improvements in technology, it is not surprising that robots are being used for the rehabilitation of patients with various medical conditions and diseases. Similarly, electromechanically assisted or robotic gait training is used for stroke patients to aid their overground gait. These devices are much more effective for both the patients and the therapist due to their automated nature. However, more research needs to be done, and the devices need to be more reasonably priced and readily available to benefit the medical industry as a whole.
Cardiorespiratory Training
Because the stroke results from a lack of oxygen for the brain, stroke survivors may require cardiorespiratory training following the attack. A stroke significantly damages the blood circulation and fluid levels throughout an individual’s body, so it is crucial to help the patient return to their previous blood circulation levels. This particular treatment involves a host of exercise programs, including overground walking, treadmill training, virtual reality training, and much more. The goal is to regulate blood flow and oxygen throughout the body and regain the blood flow and fluid levels prior to the stroke.
Have any questions regarding the topic “Stroke rehabilitation” feel free to comment below.
Also Read: Ataxia rehabilitation