Can Stress Cause a Stroke? Yes, and Here’s What You Can Do

It is natural to feel stressed. And it might seem like there’s always something more to worry about. Stress has a function, but when it lasts for an extended period of time (chronic stress), it may do more damage than good. It may also lead to significant health problems such as high blood pressure, heart disease, and strokes.
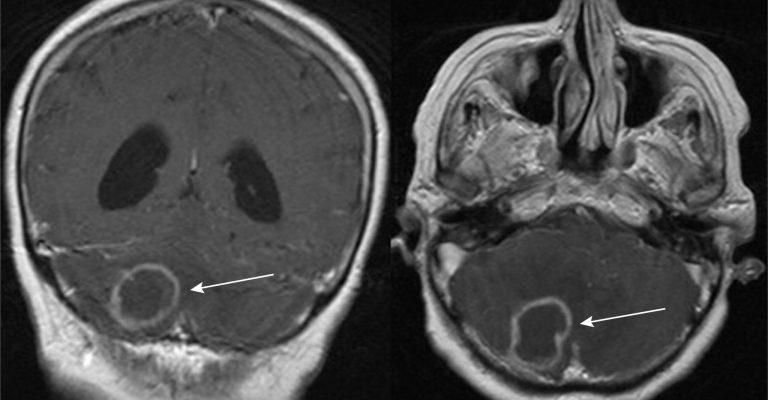
A stroke occurs when a region of the brain does not get enough blood and nutrients. Depending on which section of the brain is affected, a stroke may induce a variety of symptoms. A portion of the face or body may feel weak. A stroke may impair speech or eyesight.
You’re going to discover how can stress cause a stroke, as well as what measures you can take to minimize stress and enhance your general health.
How can stress cause a stroke?
What occurs when you are stressed relies on the other variables you are dealing with. Stress may induce medical difficulties or operate in conjunction with other medical conditions to cause a stroke.
There is often underlying damage to the circulatory system prior to a stroke, such as weakened or restricted arteries. This is where the stroke-stress relationship emerges: persistent stress may add to artery damage and raise the risk of stroke. But how precisely does it happen?
When the body is stressed, it releases stress chemicals such as cortisol. These hormones assist the body in retaining water, salt, and sugar, therefore maintaining blood pressure and ensuring the body has adequate fuel to operate.
While this is useful for dealing with stress, it may have detrimental health consequences if the body continues in this condition for an extended length of time.
A catastrophic health incident, such as a heart attack, stroke, or being diagnosed with a disease, may also be stressful. And that stress might slow down the rehabilitation process or possibly cause new health concerns.
What research reveals about stress

Increasing levels of psychological strain (such as those caused by job demands) are linked to an increased risk of both fatal and nonfatal stroke in adults.
Here are some data that address your concern about how can stress cause a stroke if it is not managed:
Blood pressure is high.
Chronic stress may weaken the arteries when it causes high blood pressure. According to 2015 research, 77% of persons who suffered their first stroke had high blood pressure.
Reactivity of blood pressure
Blood pressure reactivity occurs when blood pressure rises in response to stress. According to 2001 research, males with excessive blood pressure reactivity were 72% more likely to have a stroke. Excessive blood pressure reactivity has also been associated with atherosclerosis and hypertension, both of which are risk factors for stroke.
Habits that cause stress
According to 2012 research, people with stressful habits such as “type A personality characteristics” and “heavy use of energy-providing beverages” are at an elevated risk of stroke.
Workplace stress
Researchers in China combined data from six investigations, including 138,782 individuals, for one study. The researchers investigated the relationship between occupational stress and future stroke risk. The research, published in the journal Neurology, demonstrates that stress-related stroke is a real possibility — and that any stress is damaging to your health and should be addressed carefully.
A 2010 research found ten risk variables that are linked to 90% of the risk of specific forms of stroke. Many of these may be triggered by work-related stress, including depression, hypertension, bad eating habits, smoking, insufficient time for exercise, or alcohol addiction.
What are the symptoms of chronic stress?

Chronic stress has an impact on both the mind and the body. It causes both physical and psychological symptoms, which might impair a person’s ability to function properly in everyday life.
The intensity of these symptoms varies from person to person. The following are some of the most prevalent symptoms of chronic stress:
- Pains and aches
- Reduced energy
- Sleeping problems
- Thinking that is disorganized.
- Fatigue
- Feelings of helplessness
- Helplessness feelings
- Infections and diseases are common.
- gastrointestinal issues
- Headaches
- Irritability
- Muscle tenseness
- Anxiety and nervousness
- Concentration issues
- Stomach ache
If you recognize any of these scenarios or symptoms, you may be suffering from chronic stress.
So now, we will then look at techniques to assist manage it.
Methods for dealing with chronic stress
Because there is a significant link between stress and stroke, it is critical to identify measures to minimize stress and enhance general health.
Here are a few evidence-based stress-reduction techniques:
Improve your stress resistance.
Long-term healthy habits may also be beneficial since they can help you develop resilience and allow you opportunities to relax on a regular basis. This might help you avoid being so anxious that you don’t know how stressed you are, preventing you from taking action to minimize stress in your life. It may also protect you from the more serious consequences of prolonged stress.
Work out multiple times each week

Exercise is an effective stress-reduction strategy since it provides two advantages. For starters, exercise increases endorphins (the brain’s “feel good” chemicals) and reduces the emotional impacts of stress. Second, exercise improves cardiovascular health, therefore protecting your body from the negative impacts of stress, such as high blood pressure.
Keep an eye on your caffeine use.
A cup of coffee in the morning may be beneficial to your health, but avoid consuming too much or too late. Too much caffeine, whether from coffee, energy drinks, or other sources, may induce jittery, anxious sensations that can add to the stress. Caffeine use too late in the day may also lead to sleeplessness. Pay attention to the dose and timing of your caffeine consumption if you suffer from anxiety or sleeplessness.
Recognizing the relationship between stress and stroke
Can stress cause a stroke? YES. Chronic stress has a direct influence on the cardiovascular system, causing artery damage if left untreated. A stroke is a medical emergency caused by a blocked or ruptured artery in the brain. Vascular disease may ultimately lead to a stroke.
Chronic stress is most usually caused by the job, relationships, or financial difficulties. While we cannot always control certain circumstances, we can influence how we react to them. Selecting activities like exercise and deep breathing may help relieve stress and, as a consequence, lower your risk of stroke.