
The action of the wrist that opens and closes the fingers during tenodesis is known as the “grasp and release.” The tendons in the forearm and the fingers serve as a large pulley system since they cross over several joints.
Tenodesis function is wholly dependent on active wrist extension against gravity; nevertheless, the process of developing tenodesis function is not completely understood. Tenodesis function is wholly dependent on active wrist extension against gravity. Although a spinal cord injury is typically thought of as a condition that affects the central nervous system due to the damage that occurs to the upper motor neurons, it is not unheard of for concurrent lower motor neuron damage to occur at the level of the injury.
This is because SCI causes damage to the upper motor neurons. Recent studies have shown that damage to the lower motor neurons at the level of the lesion to the finger extensors is a robust predictor for the development of tenodesis function. The maturation of the tenodesis function may be aided in the following ways:
There have been numerous attempts at delivering the requisite tenodesis function using a variety of splinting and taping procedures, but none of these approaches have yet been demonstrated to be superior. If you don’t develop the tenodesis function in your hand, you’ll probably end up with a hand that’s less functional. The intrinsic minus is a presentation that is used rather frequently (claw hand).
When your knuckles are higher than your wrist, this position is known as wrist extension or hand grab. When you stretch your wrist, your fingers will instinctively curl or hold onto one another. When the wrist is extended, the tendons that run down the fingers become more condensed, which causes the finger joints to bend forward.
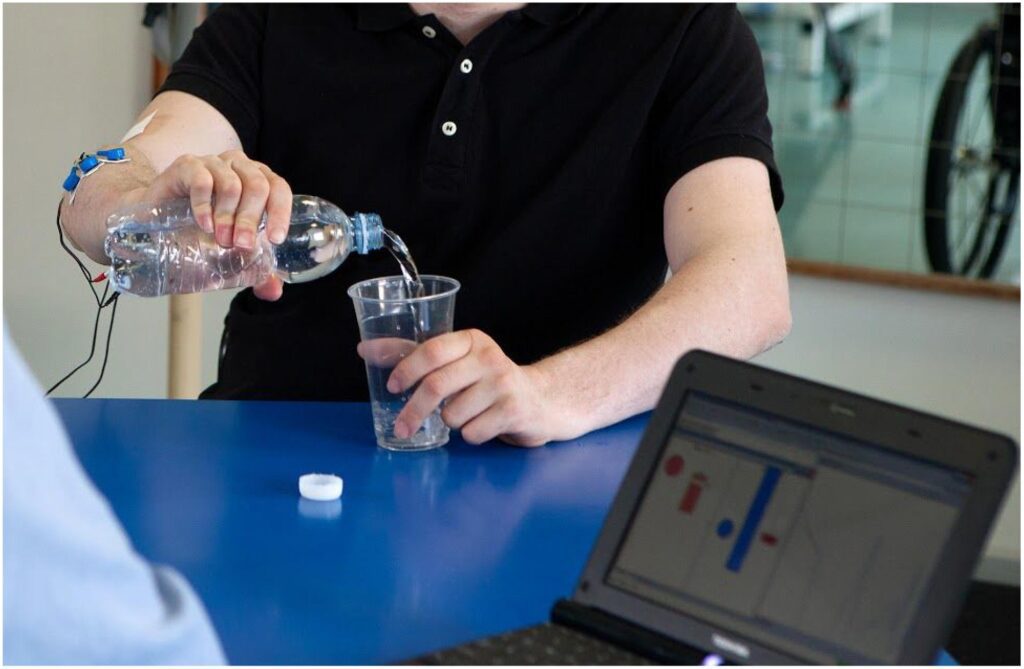
Tenodesis grip and release is a method that allows people with spinal cord injuries to pick things up, grab them, and then let go of them.
To open and close their fingers, persons who are able to do so use the flexor and extensor muscles in their hands. Signals may be sent to the muscles that control the wrist after an injury to the cervical level of the spinal cord, which is the neck. However, signals may not be sent to the muscles that control the fingers after such an injury.
When I want to keep my hand and fingers together, I utilize a wrist extender. This makes my fingers more rigid, which improves my ability to grasp objects. I release my grip on objects by flexing my wrist, which also opens up my hand and fingers, so I can let go of things without difficulty.
If I try to take up a water bottle while keeping my wrist completely straight, I won’t be able to retain it in my fingers for very long. For this reason, I grab the bottle by flexing my wrist to open my fingers, then extending my wrist to shut my fingers before picking it up. This allows me to obtain a good grip on the bottle.
If I try to pick up a packet of gloves while keeping my wrist in a flat position, I won’t have any grip. Therefore, I bend my wrist to open my fingers, and then I extend it so that I can hold the gloves while keeping my fingers closed on them.
When it’s time to dine, I can comfortably hold a fork between the index and middle fingers on either hand. In this position, I have no problems chewing my food; however, if I wish to pierce something firm, like a piece of steak, and keep my wrist straight, the fork will glide between my fingers. My fingers are able to maintain a more secure hold on the fork, though, because I extend my wrist while I hold it. After that, I’ll be able to prod the steak without the tines of the fork sliding as readily through my fingers.

If a patient has been experiencing significant discomfort and weakness in the shoulder as a result of a biceps tendon injury, tenodesis surgery may be an option for them to explore as a treatment option. This can typically be diagnosed by looking at the patient’s medical history, performing a physical examination, and performing imaging tests on the joint, such as an X-ray or an MRI scan.
In addition to this, it is possible that an arthroscopic examination of the joint will be required. Tenodesis is a procedure that can be performed on individuals of any age; however, it is most typically employed for younger patients who lead a physically active and athletic lifestyle.
Tenodesis is an outpatient surgery that can take anywhere from sixty to ninety minutes to conduct. Following the administration of general anesthesia, the first step of the tenodesis operation involves the surgeon gaining access to the joint located in the shoulder region. It is frequently carried out arthroscopically, which is a minimally invasive technique that involves making several small incisions into which a fiber-optic device and tiny surgical instruments are inserted.
This affords patients the benefits of causing less damage to the surrounding tissues and requiring less time for recovery. In some circumstances, a conventional open operation might be required. If this is the case, a single, more extensive incision will need to be made in order to gain access to the joint.
After removing any injured tissue that may have been surrounding the biceps tendon, the surgeon will then disconnect the tendon from its junction with the labrum. We will remove any bone or cartilage pieces, as well as any bone spurs, that we find have the potential to irritate the tendon. After this, anchors and sturdy sutures are used to secure the tendon’s attachment to the humerus bone around the shoulder joint. This helps to keep the tendon in its proper location. This helps to relieve some of the strain that was being exerted on the tendon as well as the labrum.
After a tenodesis operation, a patient typically does not need to spend the night in the hospital. Following shoulder surgery, patients will need to have their arms immobilized in a sling for many weeks so that the recovering shoulder joint may receive the necessary support and protection.
The recuperation process is helped by physical therapy, which helps to strengthen and restore function to the injured shoulder. The majority of patients are able to return to work in sedentary employment within a few days, but it typically takes between three and six months before they are authorized to engage in more rigorous activities.